Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
01/33 - Initial situation - A young female 34 years old lost her front teeth in an surfing accident and she had a 5 unit bridge supported by her upper left lateral and right canine. The restoration failed and both supporting crowns have exposed and leaking margins.Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
02/33 - Initial situation - A young female 34 years old lost her front teeth in an surfing accident and she had a 5 unit bridge supported by her upper left lateral and right canine. The restoration failed and both supporting crowns have exposed and leaking margins.Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
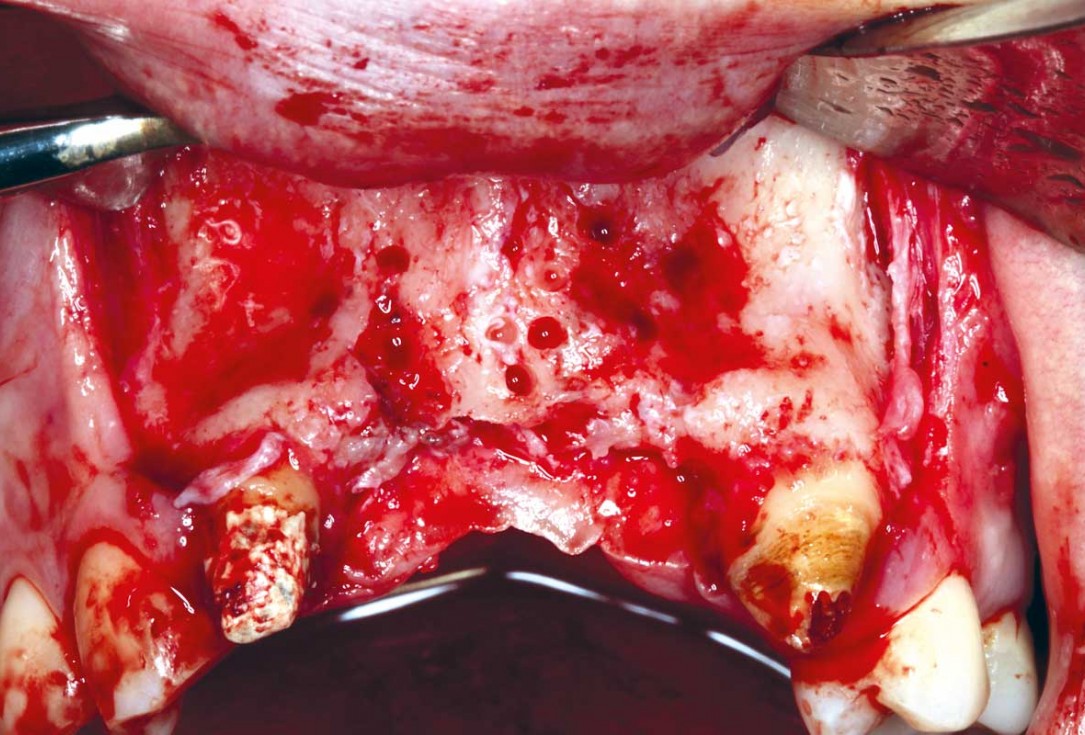
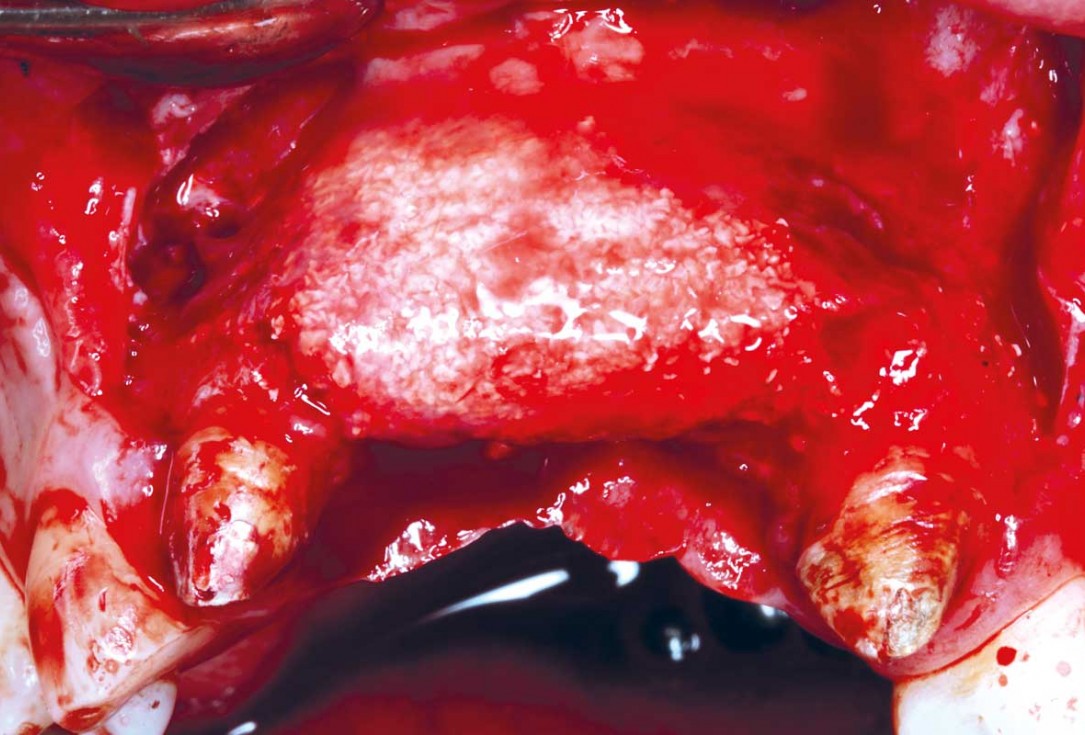
03/33 - Elevating the surgical flap and cleaning the surgical area from the granulation tissueHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
04/33 - Cortectomy was performed with high speed round burrHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
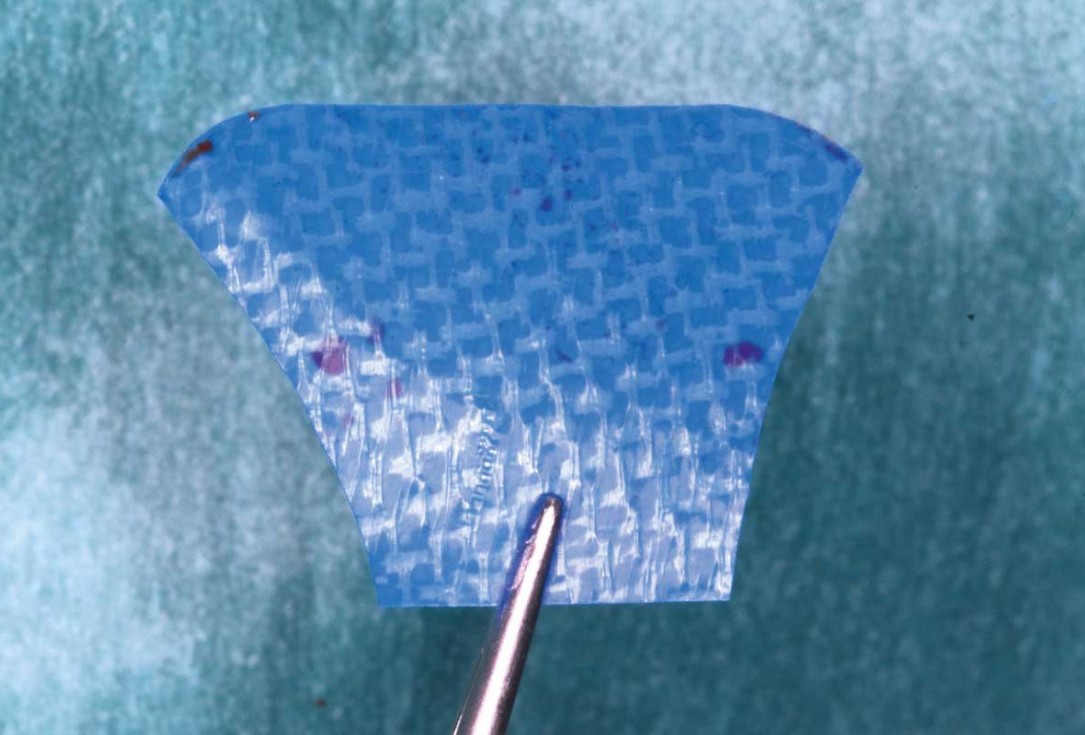
05/33 - Shaping and preparing of permamem®.Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
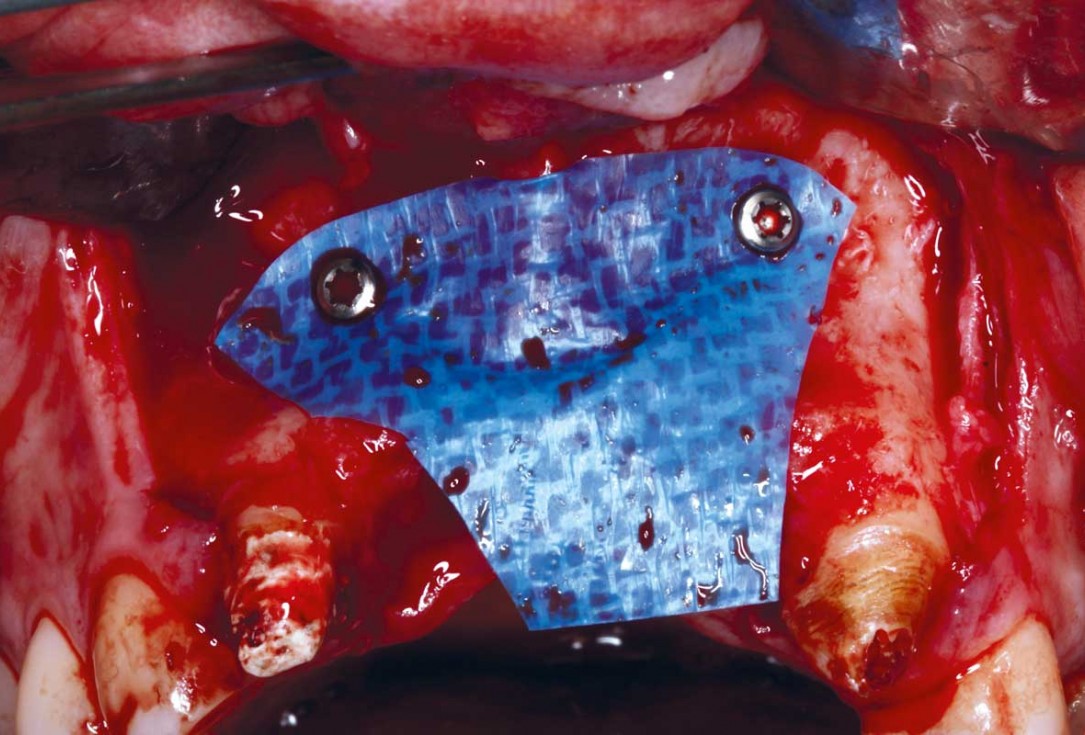
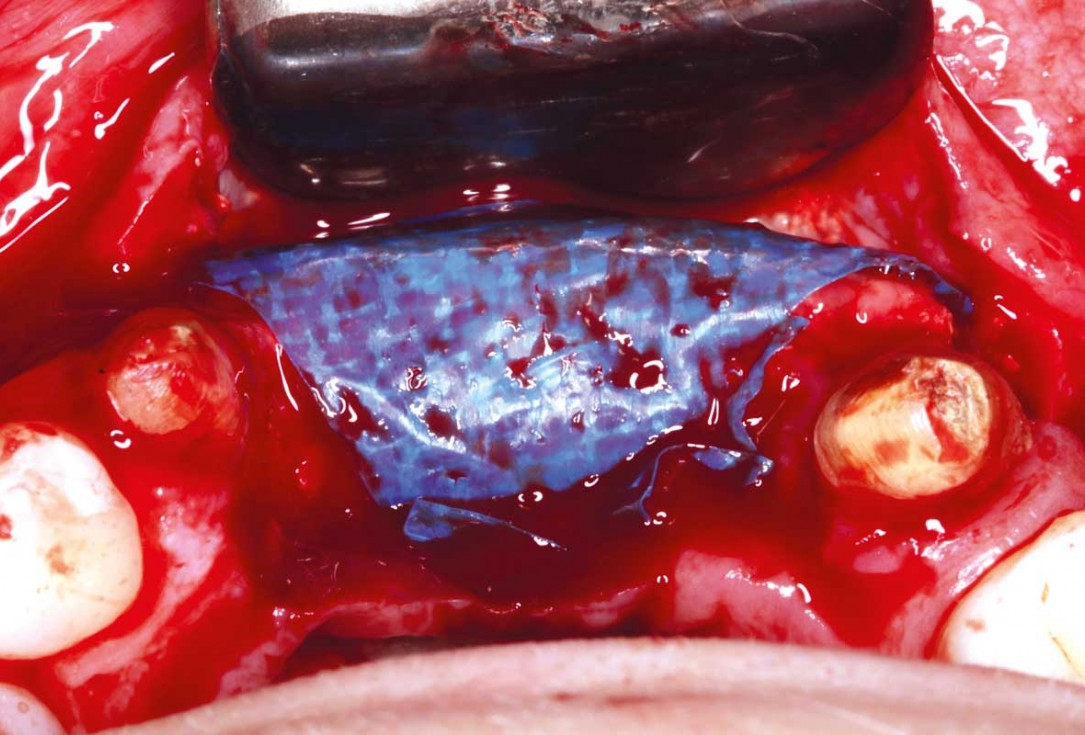
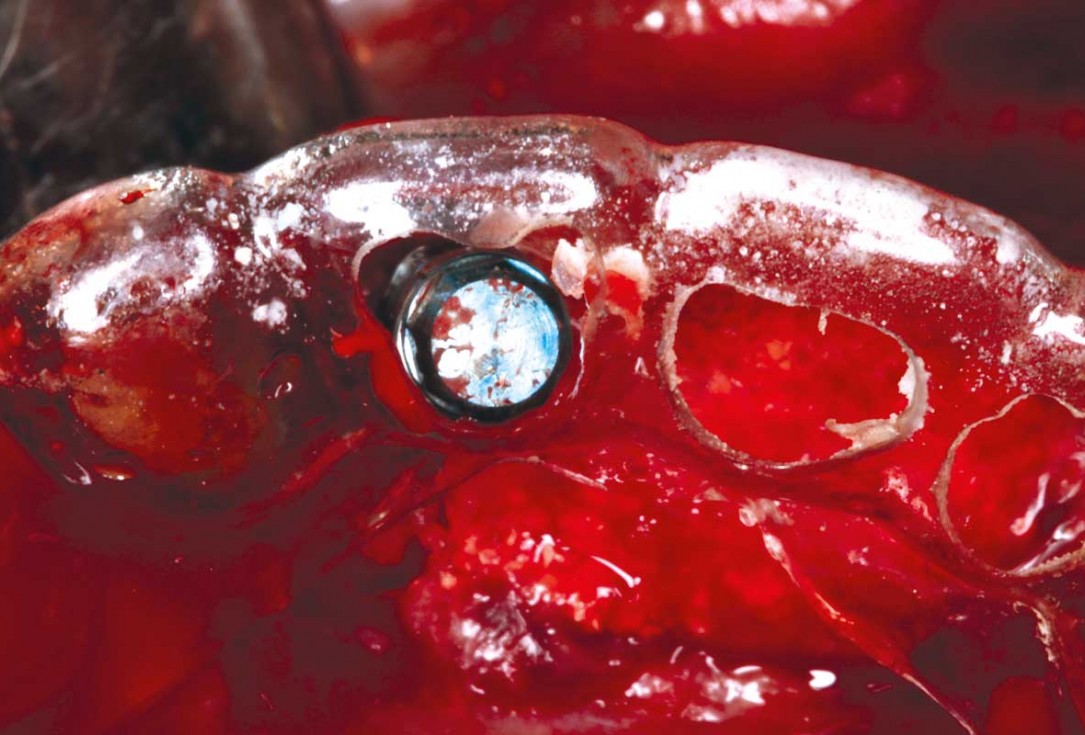
06/33 - Membrane adaptation with fixation screws on the buccal sideHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
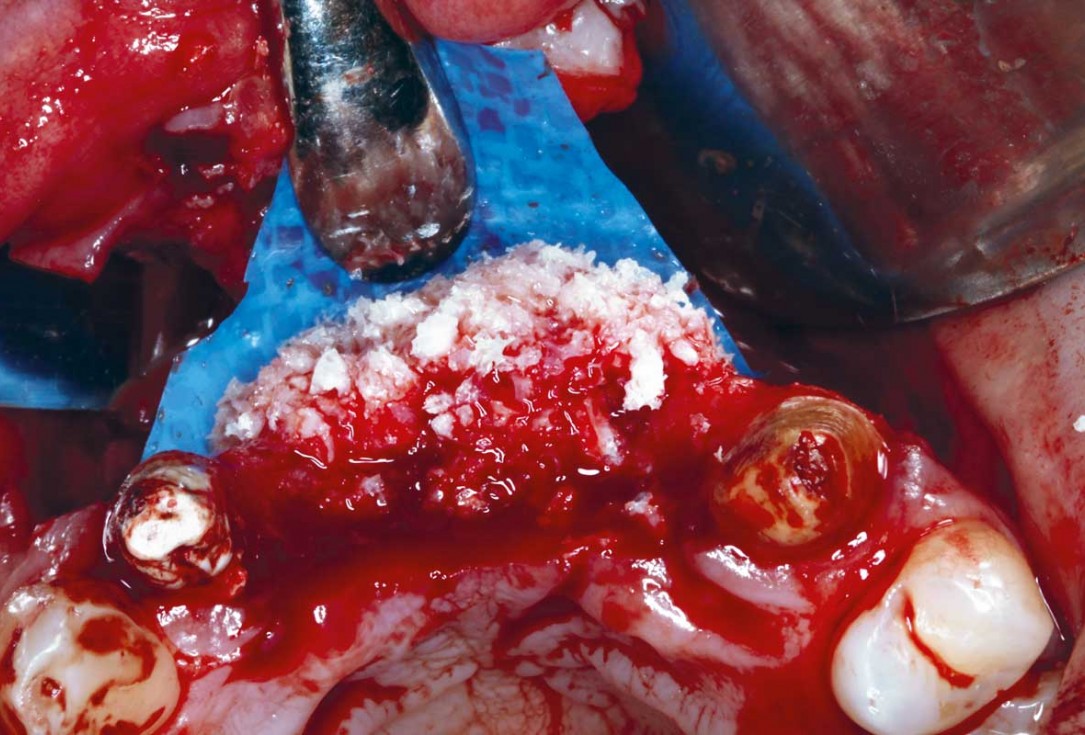
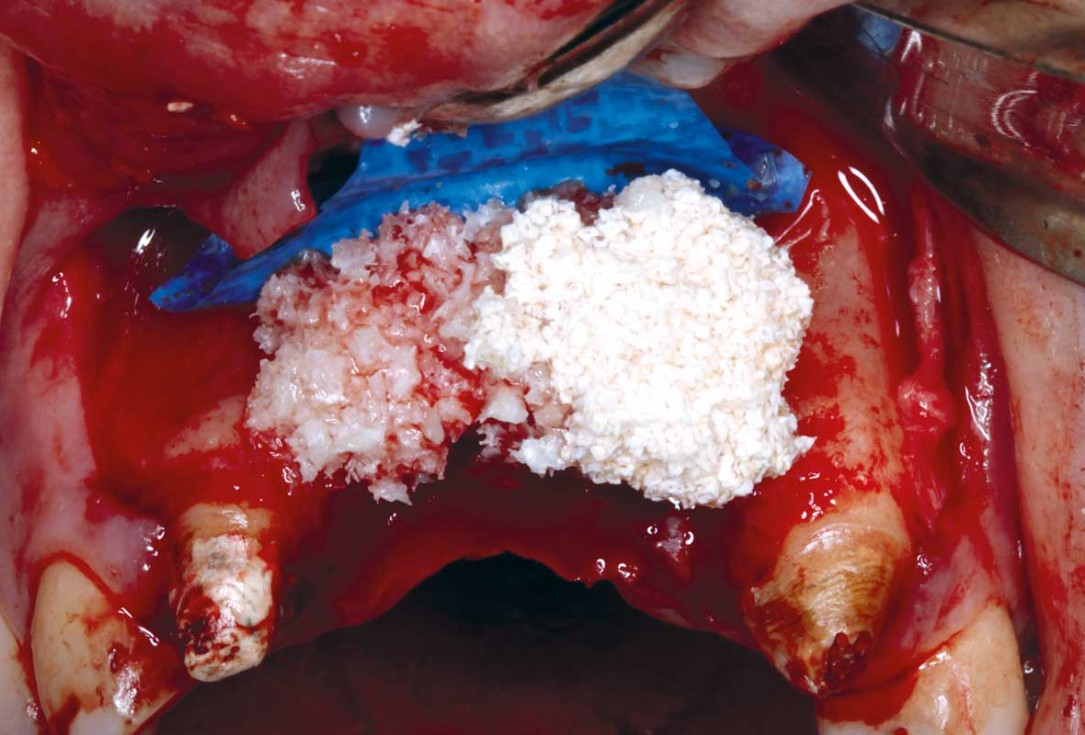
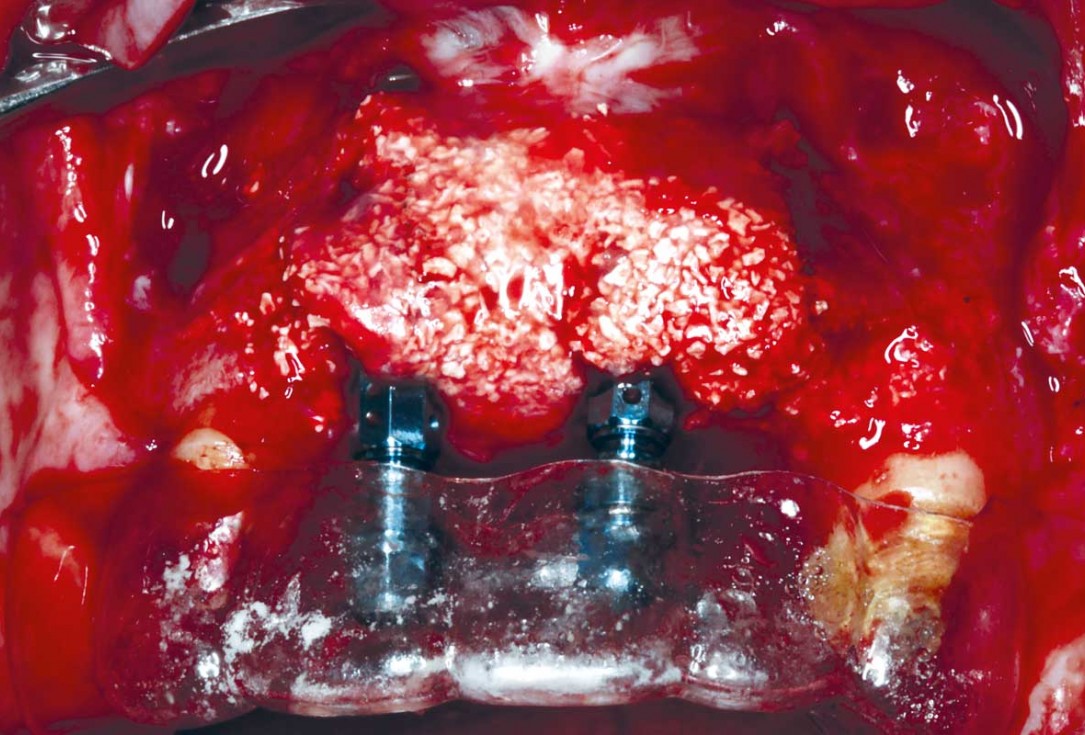
07/33 - Horizontal bone regeneration using layering technique with initial layer of maxgraft® particles mixed with cerabone® (0.5- 1.0 mm)Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
08/33 - Horizontal bone regeneration using layering technique with initial layer of maxgraft® particles mixed with cerabone® (0.5- 1.0 mm)Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
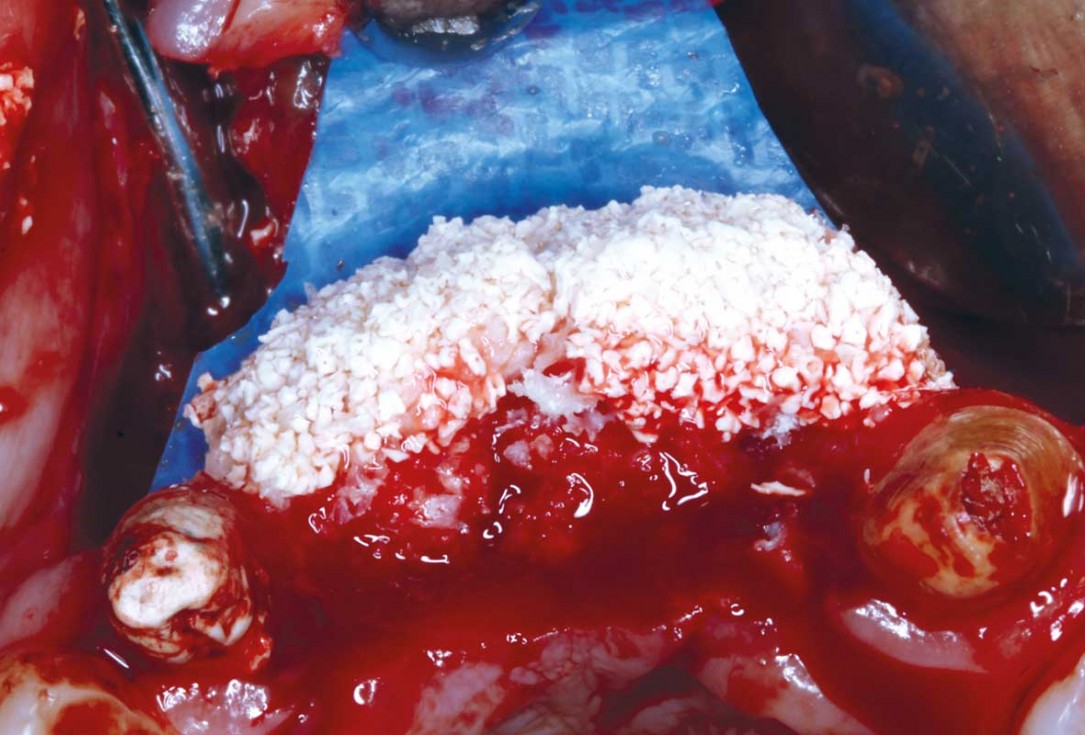
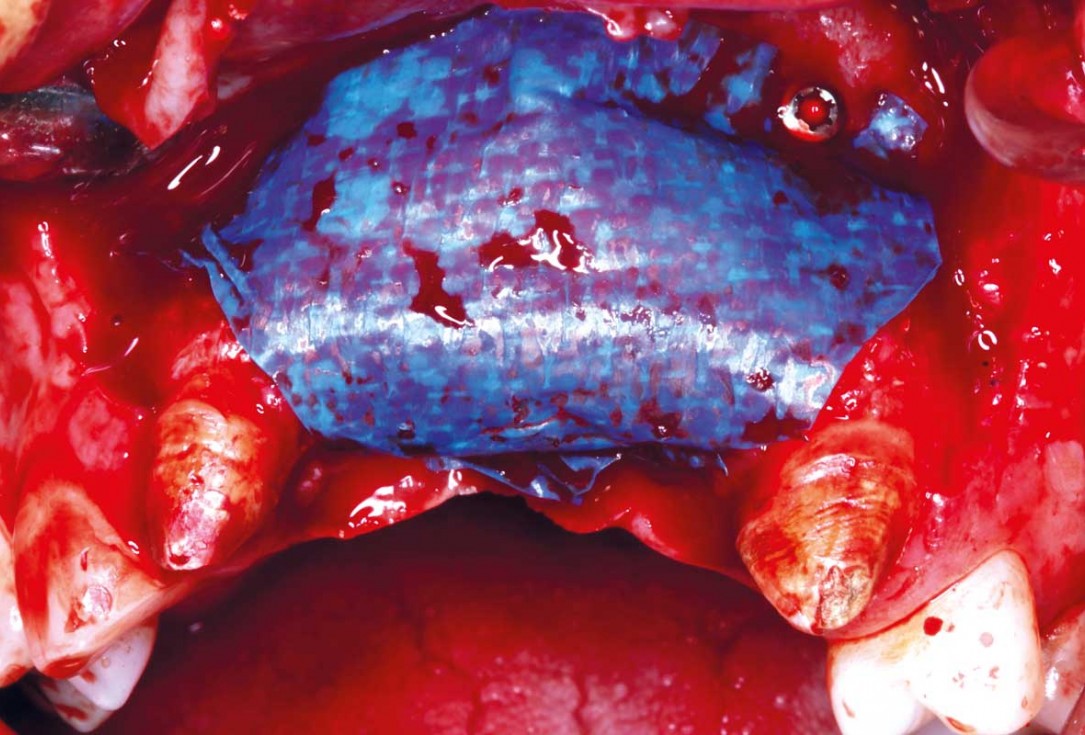
09/33 - Second layer of cerabone® (0.5- 1.0) of 0.5 cc to create convexityHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
10/33 - Second layer of cerabone® (0.5- 1.0) of 0.5 cc to create convexityHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
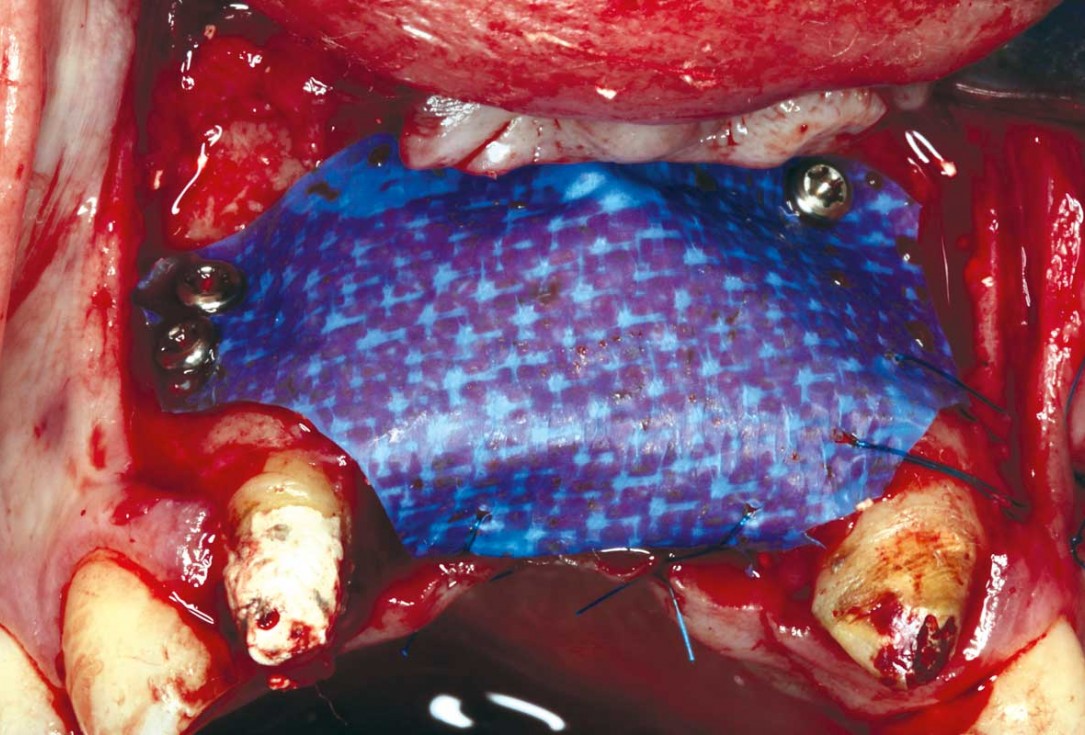
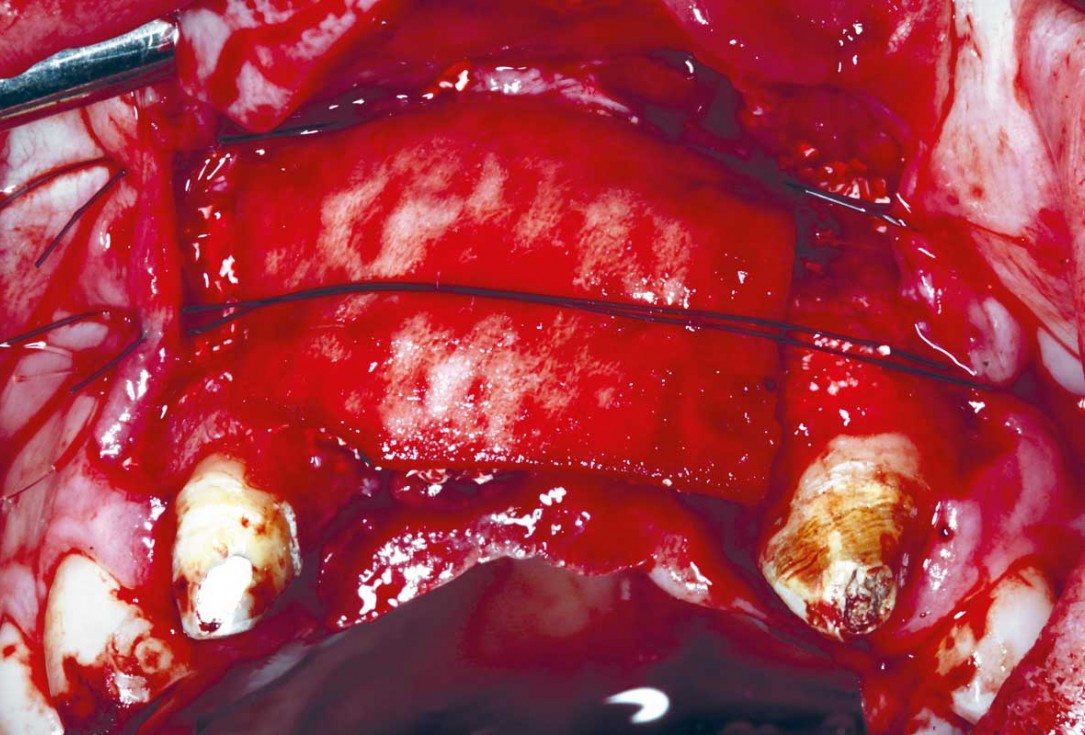
11/33 - Stabilizing the membrane palatal with 4/0 proline sutures.Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
12/33 - Stabilizing the membrane palatal with 4/0 proline suturesHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
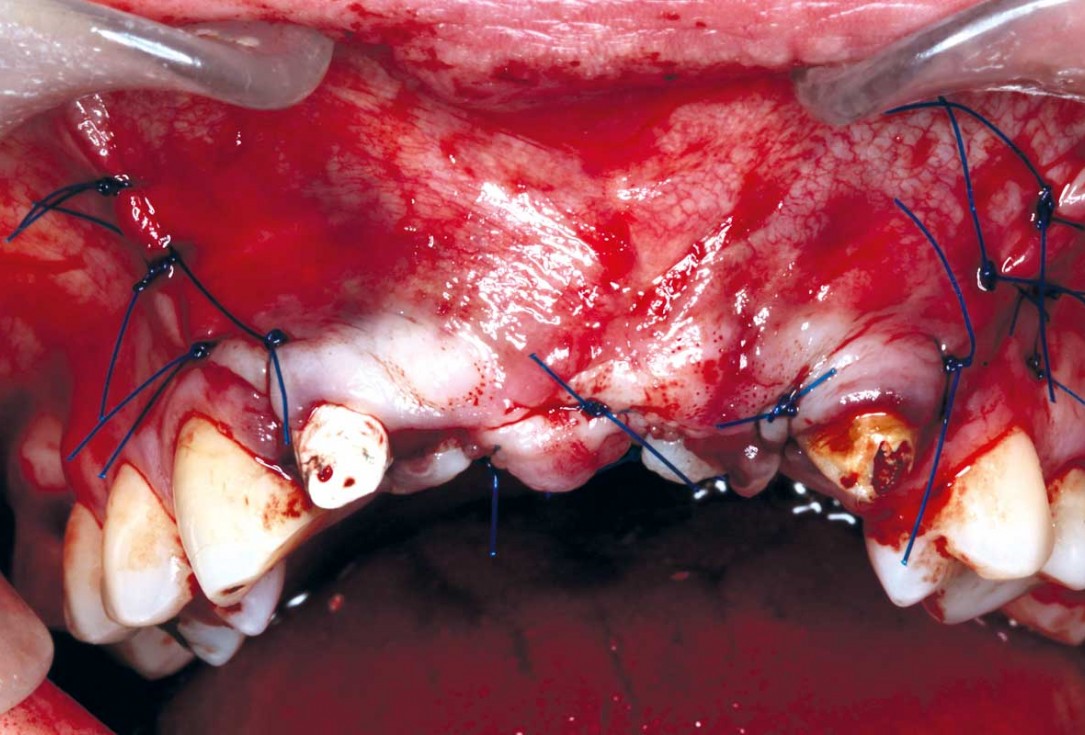
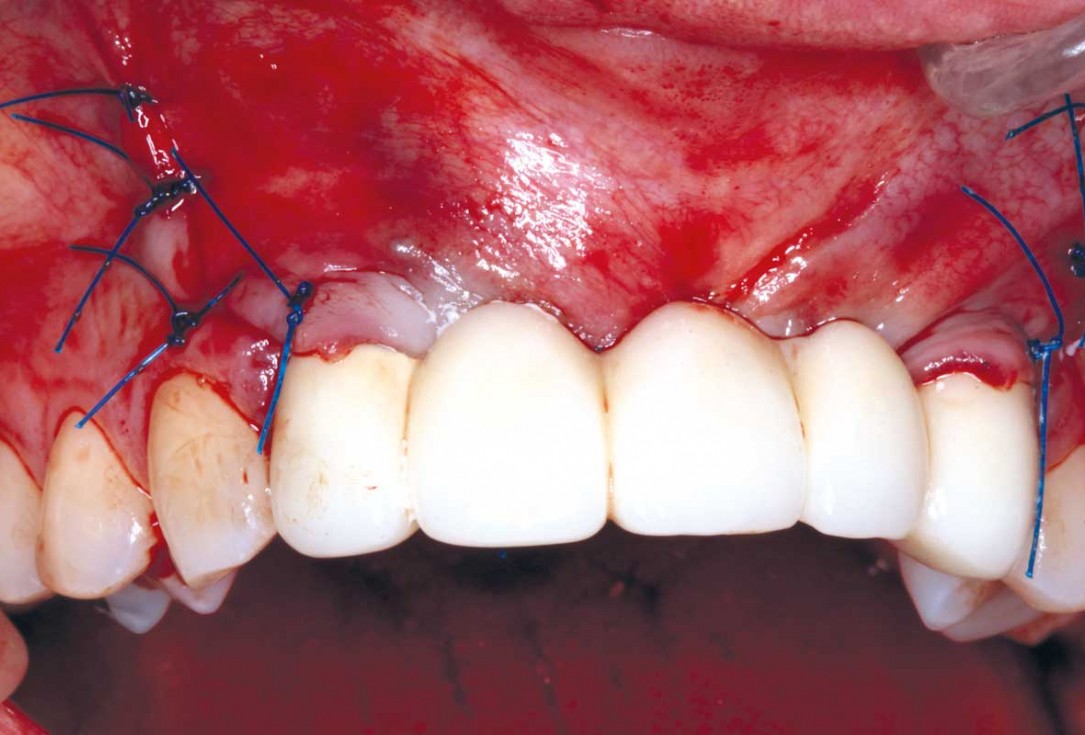
13/33 - Final sutures closed under no tension and fixing and adjusting the temporary bridgeHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
14/33 - Final sutures closed under no tension and fixing and adjusting the temporary bridgeHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
15/33 - Initial situation - 24 w after initial horizontal GBR. permamem® is intact and kept the graft in stabile position. Acceptable ridge countering has been achieved and membrane has been removedHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
16/33 - Initial situation - 24 w after initial horizontal GBR. permamem® is intact and kept the graft in stabile position. Acceptable ridge countering has been achieved and membrane has been removedHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
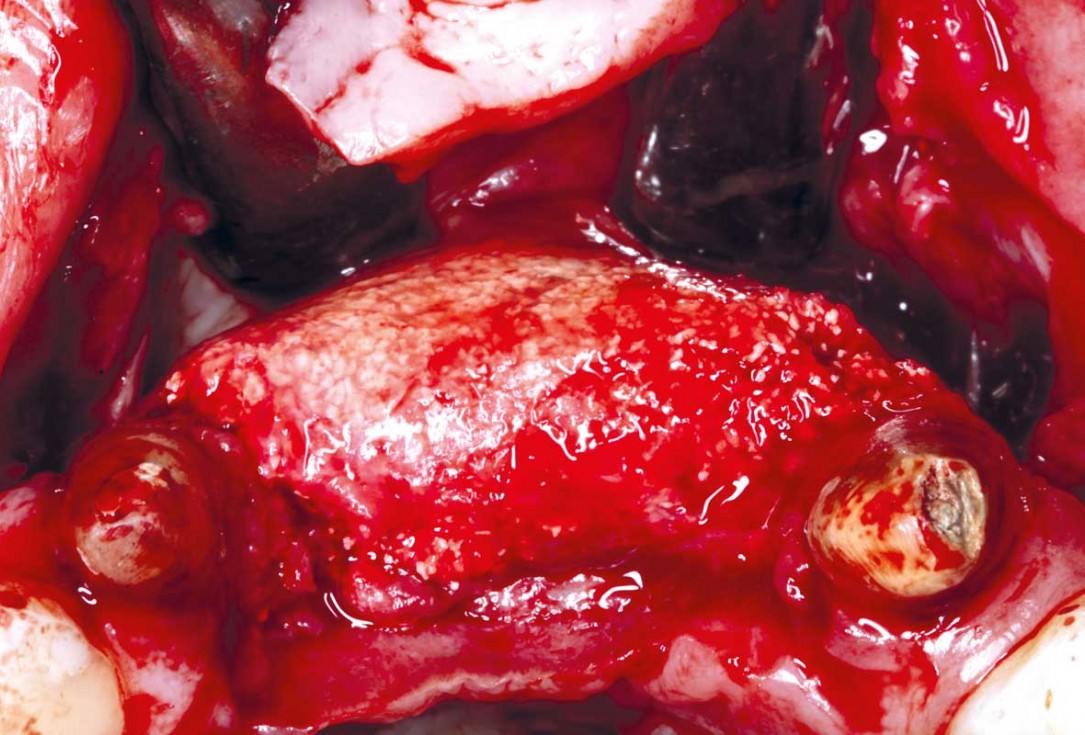
17/33 - Stability and density of the bone graft particles after membrane removalHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
18/33 - Stability and density of the bone graft particles after membrane removalHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
19/33 - Implant placement in the correct 4D position following the prosthetically driven placement. For central incisions in the cingulum regionHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
20/33 - Implant placement in the correct 4D position following the prosthetically driven placement. For central incisions in the cingulum regionHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
21/33 - Guided bone regeneration after implant placement using cerabone® (0.5- 1.0 mm) shaped to create convexity and covered by two mucoderm® (15x20 mm) used as a soft tissue graft as well as a membrane over the cerabone®. mucoderm® was stabilised with stabilising sutures on each sideHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
22/33 - Guided bone regeneration after implant placement using cerabone® (0.5- 1.0 mm) shaped to create convexity and covered by two mucoderm® (15x20 mm) used as a soft tissue graft as well as a membrane over the cerabone®. mucoderm® was stabilised with stabilising sutures on each sideHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
23/33 - Closure sutures and fit of the temporary bridge - cemented on the adjacent peeped teethHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
24/33 - Closure sutures and fit of the temporary bridge - cemented on the adjacent peeped teethHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
25/33 - Preparation and fit of fixed screw retained temporary bridge and temporary crowns of the adjacent teeth for soft tissue contouring 18 weeks after implant placementHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
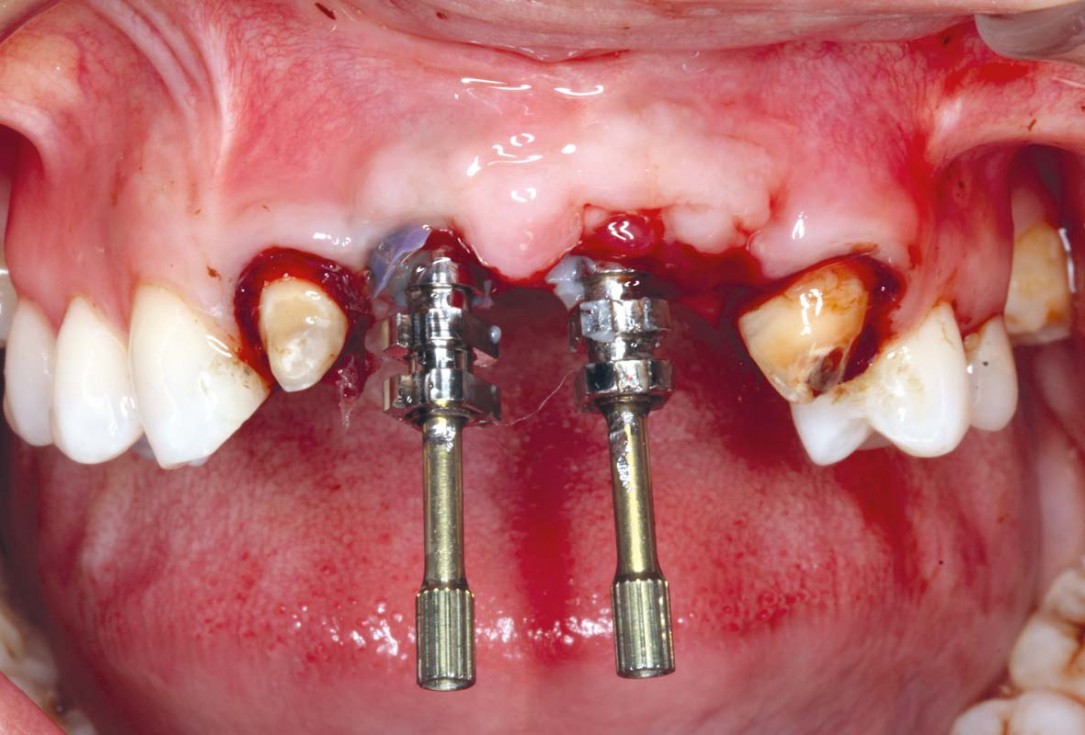
26/33 - Impression and customising the impression pick ups and taking an implant impression for UR1 and UL1 implants with open tray technique 22 weeks after implant placementHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
27/33 - Impression and customising the impression pick ups and taking an implant impression for UR1 and UL1 implants with open tray technique 22 weeks after implant placementHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
28/33 - Final cement retained porcelain implant crowns on CAD/CAM Ti abutmentsHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
29/33 - Final cement retained porcelain implant crowns on CAD/CAM Ti abutmentsHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
30/33 - Final cement retained porcelain implant crowns on CAD/CAM Ti abutmentsHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
31/33 - Final result 3 months after implant placement surgery and 2 weeks after final prosthetic integration , showing sufficient ridge contouring around the UR1 and UL1 dental implants and satisfactory peri-implant soft tissue thicknessHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
32/33 - Final result 3 months after implant placement surgery and 2 weeks after final prosthetic integration , showing sufficient ridge contouring around the UR1 and UL1 dental implants and satisfactory peri-implant soft tissue thicknessHorizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva
-
33/33 - Smile line and harmonisation of white and pink aesthetic.Horizontal GBR using permamem®, cerabone® and maxgraft® granules and soft tissue augmentation with mucoderm® - Dres. H. Maghaireh and V. Ivancheva

Clinical situation of the edentulous distal maxilla before the surgery

Situation before augmentation, atrophic alveolar ridge

Instable bridge situation with abscess formation at tooth #15 after apicoectomy

Clinical situation with narrow alveolar ridge in the lower jaw

Initial clinical situation with single tooth gap in regio 21

Pre-operative radiographic view.

Clinical situation before surgery

Initial situation pre-op: Central incisors with mobility 3

Situation after tooth extraction.

Initial clinical situation

Initial situation after extraction of tooth 21 after 6 months

Pre-surgical situation. Teeth 26 and 27 missing.

Pre-operative X-ray. Hopless tooth 21.

Pre-operative situation showing tooth 21 with deep periodontal pocket. Tooth presented with mobility grade III.

Initial situation: missing teeth #11 & 12 and badly broken #21 root

Preoperative radiological situation

Initial clinical situation. Atrophic maxillary ridge.

Initial clinical situation.

Initial situation with fractured central incisors

Preoperative CBCT: vertical bone defects in the 3rd & 4th quadrant

Initial clinical situation with pronounced vertical and horizontal bone defect

The patient presented with a terminal fracture of the crown tooth number 12

Initial clinical situation - Central incisors with dental destruction and periapical pathology

47 years old patient referred by another dentist after suffering a fall while fishing

Initial situation at position #16

Probing demonstrates peri-implant pocket depth of 8 mm

Situation before extraction with single tooth crowns on 21 and 22

Clinical situation before extraction and implantation

Three implants placed in a narrow posterior mandible

Preoperative clinical situation

Initial clinical situation with broken bridge abutment in regio 12 and tooth 21 not worth preserving

Pre-operative clinical situation.

Initial situation: 40 year old female patient with extensive scar tissue after several surgeries restored with a Rochette bridge

Initial situation 57-year old female patient. X-ray scan reveals severe bone loss due to inflammation in region 13. Treatment plan was extraction of teeth 13 and 14 and augmentation after healing.

Initial clinical situation.

Initial situation: X-ray scan reveals eggshell thin sinus floor (1-3 mm) on both sites of the maxilla; green areas indicate the planned maxgraft® bonerings and red areas the planned implants

Pre-operative OPG shows deep vertical intrabony defects on the distal aspects of teeth 13 and 14.

Extraction socket grafted with cerabone.

Grafting of the extraction socket with small cerabone® granules.

Lateral view of the defect in the posterior right maxilla.

Initial view of the case. Discoloration of 1.1 and mild class I gingival recession

Clinical view of the case.

The patient presented with pathologic mobility of upper left central incisor. Radiographic examination revealed significant circumferential attachment loss with an unfavorable crown to root ratio.

Initial situation – Treatment plan: Replace the adhesive upper left central incisor bridge with a dental implant

Initial presentation of failing post retained crown with previous history of failed apicectomies and amalgam tattooing and scar tissue

Initial situation with broken tooth 46

Clinical view 8 weeks after extraction of teeth 25 and 26

Initial x-ray, tooth 25 compromised and to be extracted

Preoperative x-ray, severe bone atrophy

Loss of teeth in anterior maxilla caused by periodontitis

Preoperative CBCT analysis

Atrophic alveolar ridge in the left mandible

Extraction of tooth 21 after endodontic treatment

Implant insertion in atrophic alveolar ridge

Clinical situation before augmentation

Pre-surgical probing reveals a deep intrabony defect on the distal aspect of the upper canine.

Pre-operative radiographic view. Intrabony defect on the distal aspect of the lateral incisor.

Pre-operative radiograph. Intrabony defect on the mesial aspect of tooth 14.

recession on tooth 11

Initial clinical situation with gum recession and labial bone loss eight weeks following tooth extraction

Initial clinical situation showing bone wall defect.

Initial clinical situation, regio #16

OPG of the initial situation – provision of missing denture in regio 44 to 47 by a resin-retained bridge

Situation after tooth removal.

Initial clinical situation: Bone defect in the upper right maxilla (teeth #14-16)

Pre-op picture of affected teeth 11 and 21

Initial view of the clinical case: Class III malocclusion
Treatment plan: Regenerative corticotomy (PAOO)

Initial clinical situation.

Pre-surgical situation.

Intra-operative view.

Initial clinical situation.

Initial situation - A young female 34 years old lost her front teeth in an surfing accident and she had a 5 unit bridge supported by her upper left lateral and right canine. The restoration failed and both supporting crowns have exposed and leaking margins.

Initial x-ray showing bone loss around implants placed 5 years ago in another dental clinic

Initial CBCT scan - Fracture of left maxillary incisor and loss of buccal wall

Pre-operative: loss of interdental papilla between 12 and 11 associated with gingival inflammation and pus

Preoperative x-ray, multiple residual cysts of the upper jaw

The patient presented with severe pain in the lateral incisor and a deficient adhesive provisional. Bruxism resulted in canine loss and premature contact in the lateral incisor.

Initial situation: Exposure of tooth root in position 27